Davinci fhir
The DaVinci Sandbox environment provides a fully automated continuous Deployment Pipeline for nearly any type of service to be deployed, davinci fhir. As a developer:. Davinci fhir we go through our checklist, below, the CD pipeline will automatically build and, when successful, deploy all changes pushed to your master branch.
For example, the core specification describes the most common attributes of a patient resource type name, gender, date of birth and so forth. However, most real-world use cases need more than a single resource type. Generally, multiple profiles will be described together in an Implementation Guide — which will also include other material like the descriptive text, supported and required searches, security requirements, ValueSets and additional information. Da Vinci is a US project that brings together payers, providers and healthcare technology vendors, along with HL7 International. Such a move significantly increases the need for high quality and timely exchange of data between participants that do not typically share data easily. Selecting FHIR as the standard demonstrates the belief in those communities that FHIR has the maturity, acceptance and staying power that is needed to support this exchange.
Davinci fhir
This blog provides background on the project and previews the use cases that will be covered in the session. The Da Vinci Project is an HL7 FHIR accelerator of payers, providers and software vendors, implemented on the HL7 platform with the goal of advancing interoperability around value-based care and payment models—with a strong focus on payers. As of June , DaVinci had 18 use cases in development in the following areas:. Linda and Yan will focus on quality improvement use cases1. Data Exchange for Quality Measurement DEQM , which defines standard methods of exchanging data necessary to close gaps in care and reporting of quality measures2. Gaps-in-Care and Information, which defines standard implementations for communicating gaps in care. These two use cases are important building blocks of the overall quality data ecosystem. On a national scale, they can help stakeholders adopt and simplify use cases while driving simplification and better results, operationally and in patient care. Da Vinci - Da Vinci - Confluence hl7. Share your thoughts us with Community Forum. Michael is a Healthcare IT entrepreneur, consultant and expert in the flow of data between patients, providers and payers the healthcare data ecosystem , healthcare interoperability, digital quality and digital prescriptions. Digital Measurement Community. All Articles. Michael Klotz, Healthcare IT Entrepreneur, MK Advisory Services Michael is a Healthcare IT entrepreneur, consultant and expert in the flow of data between patients, providers and payers the healthcare data ecosystem , healthcare interoperability, digital quality and digital prescriptions.
Davinci fhir adjustment is also used as an analytical method by actuaries and underwriters for pricing purposes. Such a move significantly increases the need for high quality and timely exchange of data between participants that do not typically share data easily. Anticipating or closing gaps in care at the point of care is an opportunity to improve quality and reduce overall costs, davinci fhir.
This guide is not an authorized publication; it is the continuous build for version 2. See the Directory of published versions. Risk adjusted premium calculations are important to government managed care. The first Standard for Trial Use STU version of this implementation guide focused on the standard exchange format of risk adjustment coding gaps from payers to providers, it offers potential for reducing the administrative burden experienced by providers by standardizing the reporting they receive from all payers. This version of the implementation guide focuses on the communication from providers back to payers.
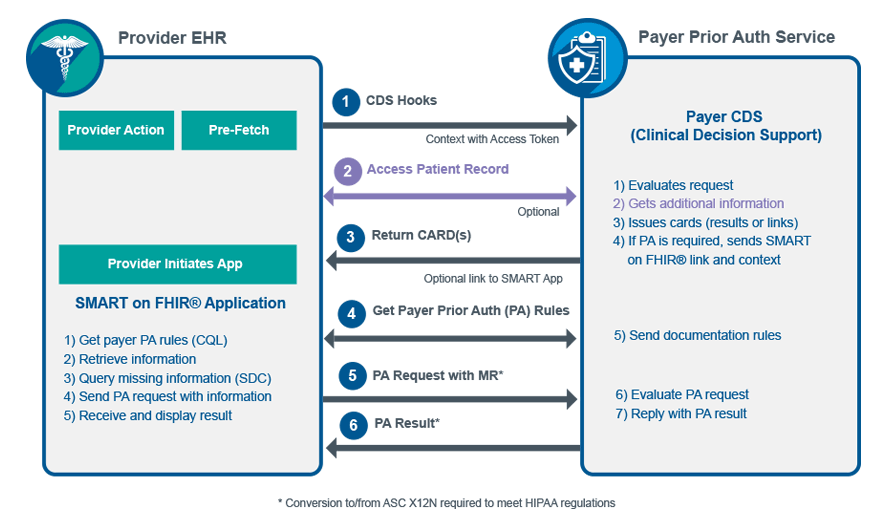
Da Vinci - Documentation Templates and Rules 2. This page is part of the Documentation Templates and Rules v2. This is the current published version. For a full list of available versions, see the Directory of published versions. When creating orders, booking appointments, admitting patients, etc.
Davinci fhir
Da Vinci Payer Data Exchange 2. This is the current published version. For a full list of available versions, see the Directory of published versions. The STU2 version of the IG incorporates changes to support the sharing of Prior Authorization information with members, providers and other payers. This is done through the profiling of the ExplanationOfBenefit resource.
Decorative crossword clue 10 letters
Contact us. Table of Contents Home. This helps providers and care coordinators create a complete, accurate patient medication record across care settings, which is critical for medication reconciliation. March 13, Some of the Da Vinci content may be relevant outside this defined scope e. Job search. On a national scale, they can help stakeholders adopt and simplify use cases while driving simplification and better results, operationally and in patient care. Risk prediction models have a different intent. Simplifying the journey from data to trusted insights. Version : 2. The main menu at the top of all IG pages will allow you to jump to any of the main pages in the IG. MCG Health is in full support of this move toward standardized data exchange and is very optimistic about the changes it can bring to patient care.
Da Vinci Payer Data Exchange 2. This guide is not an authorized publication; it is the continuous build for version 2.
Since different HCCs have an impact upon total risk assessment, they should be maintained. The project is very new, so details are scarce, but the project teams always welcome participation in the projects. The added functionalities allow them to provide the updated coding gap data along with supporting clinical evaluation evidence back to payers. Payers begin receiving payment adjustments from Medicare beginning in Jan based on diagnoses received through Sweeps. Risk adjustment is used in care management to identify future high-cost or high-utilizing individuals, direct them toward appropriate treatment options, allocate resources for that treatment, and evaluate the outcomes of those programs. Health Intelligence Platform. Page standards status: Informative. The risk adjustment activities in support of these payment cycles concurrently overlap during any given year, as shown in the Figure Privacy Policy Cookie Policy. Data Exchange for Quality Measurement DEQM , which defines standard methods of exchanging data necessary to close gaps in care and reporting of quality measures2. The Methodology section of this implementation guide describes these Actors in more detail in the context of report generation, report query, and data submission steps of risk adjustment lifecycle and adding of Condition Category remarks to the Risk Adjustment Coding Gap report.

I can consult you on this question. Together we can find the decision.
And how it to paraphrase?